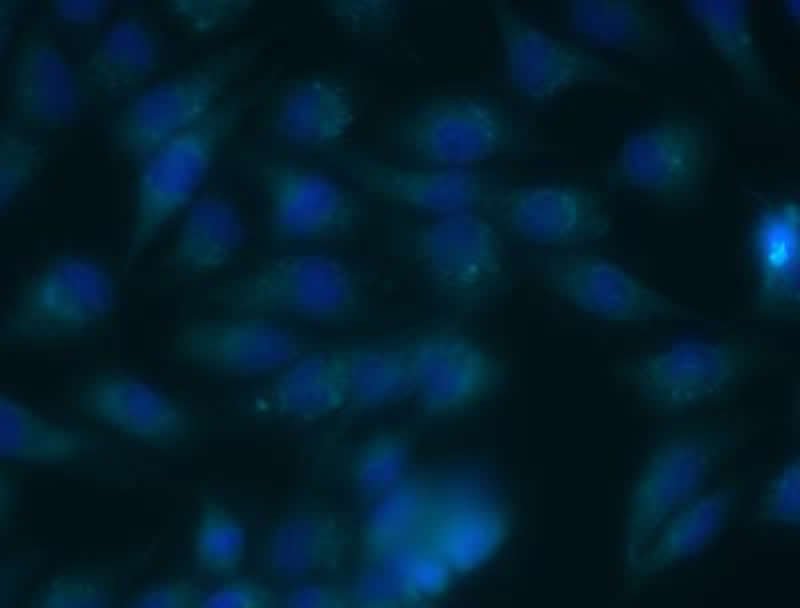
Summary: Cannabidiol (CBD) appears to slow the growth of glioblastoma brain cancer cells in both animal and human cell lines. CBD’s anti-cancer actions target mitochondria, causing them to dysfunction and release harmful reactive oxygen species. Cancer cells treated with CBD exhibited significant decreases in mitochondrial activity.
Source: Experimental Biology
Findings from a new study examining human and canine brain cancer cells suggest that cannabidiol could be a useful therapy for a difficult-to-treat brain cancer. Cannabidiol, or CBD, is a non-psychoactive chemical compound derived from marijuana.
The study looked at glioblastoma, an often-deadly form of brain cancer that grows and spreads very quickly. Even with major advancements in treatment, survival rates for this cancer have not improved significantly.
“Further research and treatment options are urgently needed for patients afflicted by brain cancer,” said Chase Gross, a student in the Doctor of Veterinary Medicine/Master of Science program at Colorado State University. “Our work shows that CBD has the potential to provide an effective, synergistic glioblastoma therapy option and that it should continue to be vigorously studied.”
Mr. Gross was scheduled to present this research at the American Society for Pharmacology and Experimental Therapeutics annual meeting in San Diego this month. Though the meeting, to be held in conjunction with the 2020 Experimental Biology conference, was canceled in response to the COVID-19 outbreak, the research team’s abstract was published in this month’s issue of The FASEB Journal.
Mr. Gross and colleagues examined human and canine glioblastoma cells because the cancer shows striking similarities between the two species. They tested the effects of CBD isolate, which contains 100 percent CBD, and CBD extract, which contains small amounts of other natural occurring compounds such as cannabigerol and tetrahydrocannabinol, or THC.
“Our experiments showed that CBD slows cancer cell growth and is toxic to both canine and human glioblastoma cell lines,” said Mr. Gross. “Importantly, the differences in anti-cancer affects between CBD isolate and extract appear to be negligible.”
The new work revealed that the toxic effects of CBD are mediated through the cell’s natural pathway for apoptosis, a form of programmed cell death. The researchers also observed that CBD-induced cell death was characterized by large, swollen intracellular vesicles before the membrane begins to bulge and breakdown. This was true for all the cell lines studied.
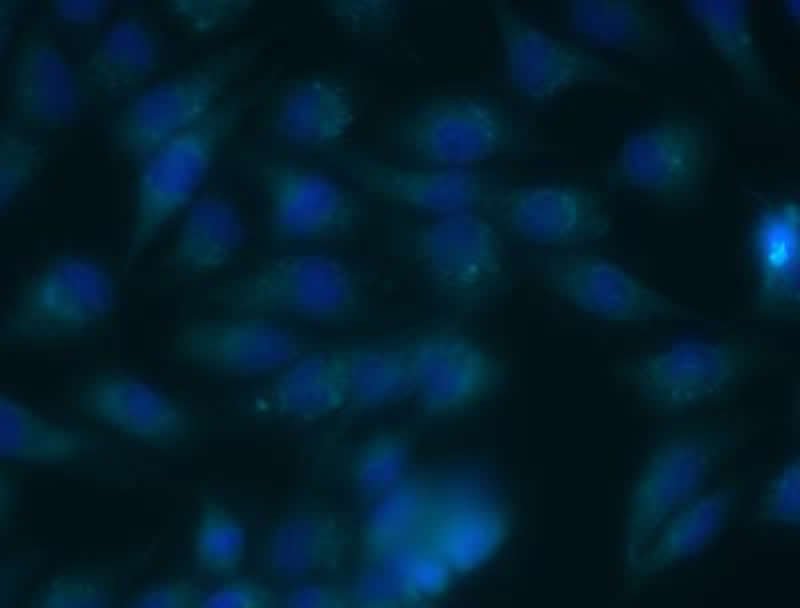
The researchers believe that CBD’s anti-cancer actions target mitochondria–the cell’s energy producing structures–by causing the mitochondria to dysfunction and release harmful reactive oxygen species. Their experiments showed that cells treated with CBD exhibited significant decreases in mitochondrial activity.
“CBD has been zealously studied in cells for its anticancer properties over the last decade,” said Mr. Gross. “Our study helps complete the in vitro puzzle, allowing us to move forward in studying CBD’s effects on glioblastoma in a clinical setting using live animal models. This could lead to new treatments that would help both people and dogs that have this very serious cancer.”
Next, the researchers plan to transition from cell cultures to animal models to test CBD’s effects on glioblastoma. If the animal studies go well, the work could progress to clinical trials on dogs that are being treated for naturally occurring glioblastoma at the Colorado State University Veterinary Teaching Hospital.
About this brain cancer research article
Source:
Experimental Biology
Media Contacts:
Anne Frances Johnson – Experimental Biology
Image Source:
The image is credited to Chase Gross, Mando Ramirez, Jade Kurihara, Colorado State University.
Original Research: The study will be presented at Experimental Biology 2020.
Feel Free To Share This Brain Cancer News.
Source: neurosciencenews.com